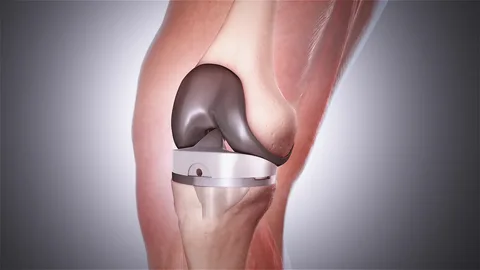
Total knee arthroplasty, commonly referred to as a total knee replacement or TKA, is a surgical procedure that resurfaces the weight-bearing surfaces of the knee joint which have been damaged as a result of osteoarthritis or other joint injuries. This involves removing the damaged surfaces of the femur, tibia, and patella and replacing them with artificial metal and plastic components. For many patients suffering from severe knee pain and loss of mobility, TKA can offer pain relief and help them regain an active lifestyle.
What happens during a TKA surgery?
The surgery for a total knee replacement is usually done under general or spinal anesthesia in a hospital operating room. Patients are advised not to eat or drink anything for at least six hours before the surgery. Once the anesthesia takes effect, the surgeon makes an incision on the front of the knee, usually 8-12 inches long. They then remove the damaged cartilage surfaces of the knee and reshape the ends of the femur and tibia to make room for the artificial knee implants.
Metal alloy components are implanted on the femur and tibia to replace the worn bone surfaces. Polyethylene plastic spacers are inserted between the metal components to replicate the cushioning function of cartilage. The surgeon also resurfaces the back of the kneecap (patella) and implants a plastic button if it shows signs of wear. The incision is carefully stitched up once the implants are securely anchored in place using bone cement.
Post-surgical care and rehabilitation
After surgery, patients are monitored in the recovery room for a few hours before being shifted to the general ward or discharged home. Cold therapy and light compression bandages are applied to reduce pain and swelling. Physical therapy begins right away with gentle range-of-motion exercises. Patients are encouraged to bear weight on the new joint as soon as pain allows, usually within a few days.
Crutches or a walker may be required initially for stability and balance as strength returns to the muscles. Most people can walk short distances unsupported within 4-6 weeks. Strengthening and flexibility exercises progress gradually over 3-6 months of physical therapy sessions. Driving may resume when patients feel confident of full control after discussion with their surgeon, usually 4-6 weeks post-op. Full recovery usually takes anywhere between 3 to 6 months.
Benefits of total knee arthroplasty
The main goals of TKA are to reduce knee pain, correct deformity, and improve mobility and function. Studies have found it to be a highly successful procedure with significant benefits:
– Pain relief – Around 90% of patients experience complete or near complete relief from knee pain after surgery.
– Regaining mobility – Most people can straighten and bend their knee almost fully after recovery. Daily activities like walking, climbing stairs, and getting in/out of chairs and cars become easier.
– Improved quality of life – Restored function and independence allows patients to resume active lifestyles and participate in sports and hobbies that were previously limited by their joint condition.
– Longevity of implants – Modern implants are designed to last 15-20 years on average. Some people need revisions later if components loosen or wear out over many years.
– Return to normal activities – Within 6 months of therapy, the majority of TKA recipients report that they have returned to enjoying daily and recreational activities like swimming, golf, cycling etc. without pain or limitations.
– Possible pain relief for other joints – Relieving stress on the knee can ease strain on neighboring hip or ankle joints that were compensating for an arthritic knee.
However, while total knee replacements can resolve knee arthritis symptoms very effectively, they do not restore normal function completely. Patients should still expect some limitations compared to healthy young knees. Outcomes also depend on factors like age, general health, pre-op range of motion, and adherence to post-op management plans.
Risks and considerations
As with any major surgery, there are certain risks involved with Total Knee Arthroplasty:
– Infection – Risk of post-surgical infection is approximately 1-2%, requiring antibiotics or repeat surgery to treat.
– Stiffness – Some temporary or even long-term limitation of knee bending may occur if stiffness develops. Early and aggressive physical therapy helps prevent this.
– Blood clots – Deep vein thrombosis or pulmonary embolism occurs in 1-2% cases without preventive measures like compression stockings and blood thinners.
– Implant failure – Components can loosen, wear out, or fracture over very long term use necessitating revision surgery in 5-10% people after 10-15 years.
– Continued pain – A small number of patients may still have some residual discomfort which therapy cannot fully alleviate.
– Anesthetic complications – Rare risks apply as with any surgery under general/epidural anesthesia including reaction to medications.
Considering the potential risks and lifetime limitations versus non-surgical options, orthopedic surgeons only recommend TKA surgery for appropriate candidates with severe knee arthritis unresponsive to other treatments. Contraindications include active joint infection, vascular disease affecting wound healing, and psychological conditions impacting rehabilitation. Overall, total knee replacement surgery has consistently proven to significantly enhance quality of life for millions of patients worldwide affected by advanced knee arthritis.
*Note:
1.Source: Coherent Market Insights, Public sources, Desk research
2.We have leveraged AI tools to mine information and compile it