Cervical cancer continues to be a prevalent issue affecting women globally, with thousands being diagnosed and losing their lives to the disease each year. While HPV vaccines offer prevention against this cancer, established cases remain challenging to treat once they progress to a metastatic or relapsing stage. However, a recent breakthrough study by a research team at Juntendo University School of Medicine in Japan has introduced a potential game-changer in the form of rejuvenated cytotoxic T lymphocytes (rejTs) for the treatment of cervical cancer.
Led by Chief Professor Miki Ando, the team, which included graduate student Yoshiki Furukawa and Assistant Professor Midori Ishii, published their findings in Cell Reports Medicine. The researchers focused on developing rejTs from induced pluripotent stem cells (iPSCs) to target specific HPV antigens found in cervical cancer cells, offering a personalized form of immunotherapy. While the ideal scenario involves using iPSCs from the patient, this approach is often impractical due to time and cost constraints.
To address the challenges associated with allogeneic iPSC-derived rejTs, the team employed CRISPR-Cas9 gene editing on HPV-specific cytotoxic T lymphocyte clone-derived iPSCs. Through a two-step gene editing process, they first removed all HLA class I antigens from the cells to evade detection and rejection by the recipient’s immune system. The second step involved introducing limited expression of HLA-A24 and HLA-E antigens to prevent attacks from natural killer (NK) cells.
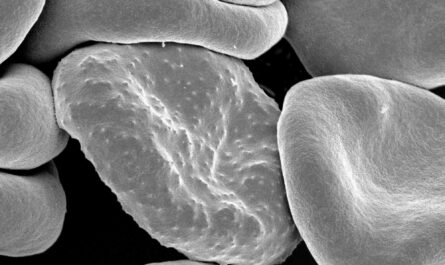
The modified iPSCs were then differentiated into T lymphocytes, which were tested for their effectiveness in fighting cervical cancer cells in both laboratory and animal models. The gene-edited rejTs demonstrated strong cytotoxicity against tumor cells while evading immune responses, leading to improved survival rates and reduced tumor growth in mice. Further analysis revealed that the rejTs were enriched with tissue-resident memory T cells, providing enhanced protection in the cervical mucosa.
The study highlighted the potential of HLA-engineered HPV-rejTs as a promising ‘off-the-shelf’ therapy for cervical cancer. Prof. Ando emphasized the sustainable approach this method offers for successful T cell therapy, signaling a significant step forward in the fight against this prevalent form of cancer. The team aims to initiate an investigator-led clinical trial in 2024 to further explore the therapeutic effects of these rejTs.
In conclusion, this pioneering research opens new possibilities in the treatment of cervical cancer and underscores the potential of gene-edited lymphocytes in revolutionizing cancer therapies.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it