A recent study conducted by the University of Gothenburg has identified a mechanism behind the development of type 2 diabetes in individuals with obesity. The research highlights the disrupted function of cleaning cells in the body as a potential explanation for why some people with obesity develop the disease while others do not.
While it is widely recognized that obesity increases the risk of insulin resistance and type 2 diabetes, the reasons for the differences in susceptibility among individuals have remained unclear. The study suggests that these variations may be related to the function of adipose tissue, rather than the amount of body fat.
The research, published in the journal PNAS, primarily focused on experiments conducted on mice, but the findings suggest that the newly discovered mechanism may also apply to humans.
During weight gain, the breakdown of collagen, a structural protein, increases to accommodate the growth of fat cells within adipose tissue. Collagen is a natural building block in the body that provides strength to cartilage, muscles, and skin.
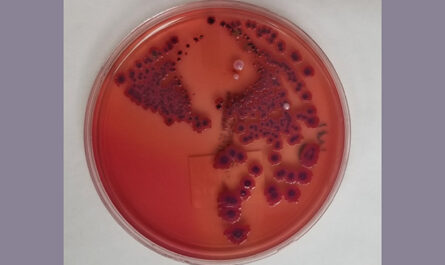
Macrophages, a type of white blood cell involved in the body’s immune response, are responsible for the breakdown of collagen. While macrophages typically aid in the destruction of invading bacteria, they also engulf and digest damaged cells and debris, such as degraded collagen, in adipose tissue during weight gain. The breakdown of collagen occurs through enzymatic degradation outside the fat cells, after which macrophages then engulf the collagen fragments for complete degradation. The study highlights the importance of the tightly regulated uptake of collagen fragments by macrophages.
However, the researchers discovered that this function of macrophages is deactivated in instances of obesity and insulin resistance, resulting in the accumulation of collagen fragments in adipose tissue.
Although this had not been considered a problem previously, the study reveals that collagen fragments actively influence various cellular processes, including inflammation and cell division, as opposed to being mere debris.
The process thus transitions from maintaining normal adipose tissue function during weight gain to becoming pathogenic in certain cases. When human macrophage samples were exposed to conditions resembling diabetes, they also lost their ability to effectively eliminate collagen.
The study was led by Ingrid Wernstedt Asterholm, a Professor in Physiology at the Sahlgrenska Academy, University of Gothenburg.
Asterholm explains that when adipose tissue expands, macrophages play a role in remodeling the tissue in a controlled manner. The reasons behind the deactivation of this mechanism are yet to be determined, but Asterholm suggests that it may occur at a genetically determined degree of adiposity.
The researchers hope that these findings will eventually lead to new strategies for the prevention and treatment of type 2 diabetes. Additionally, certain collagen fragments could potentially serve as measurable biological markers, aiding in the identification of individuals at a higher risk of developing the condition.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it